PSC
- related: GI, PBC primary biliary cholangitis
- tags: #GI
Primary Sclerosing Cholangitis
Primary sclerosing cholangitis (PSC) is an autoimmune fibroinflammatory disease of the large bile ducts, but it can also affect the small bile ducts (small-duct PSC). It is more common in men than in women, which is unique among the autoimmune liver diseases. PSC is associated with inflammatory bowel disease (IBD) in about 85% of cases; up to 7.5% of patients with ulcerative colitis have PSC.
All patients with PSC and without known IBD should have a colonoscopy at the time of PSC diagnosis. Patients with concomitant IBD may have a unique PSC-IBD phenotype, characterized by rectal sparing, mild pancolitis, and backwash ileitis; this carries a higher risk for colon cancer, requiring colonoscopy with surveillance biopsies every 1 to 2 years, as well as a higher risk for pouchitis after total colectomy.
Patients with PSC have a 15% lifetime risk for cholangiocarcinoma and also have an increased risk for gallbladder cancer. Surveillance for cholangiocarcinoma with CA 19-9 and ultrasonography or, preferably, MRCP should be completed every 6 to 12 months. The incidence of cholangiocarcinoma is highest in the first 2 years after diagnosis of PSC is made.
The diagnosis of PSC can be made noninvasively through MR cholangiopancreatography (MRCP) (Figure 31). Endoscopic retrograde cholangiopancreatography (ERCP) should be considered in patients with jaundice, worsening pruritus, bacterial cholangitis, or a dominant stricture or bile duct mass seen on MRCP. Symptoms of bacterial cholangitis, increasing jaundice, and pruritus can signify strictures that may improve with dilation or stenting, or, alternatively, removing sludge or stone debris in the bile ducts via ERCP. A dominant stricture in a patient with PSC must be evaluated for cholangiocarcinoma by obtaining biliary brushings for cytologic examination, and, if available, fluorescent in situ hybridization to evaluate chromosomal abnormalities. Diagnosis of PSC does not usually require liver biopsy; small-duct PSC, which cannot be diagnosed by MRCP, is an exception.
- MR cholangiopancreatography (MRCP) is often the imaging of choice due to its noninvasive nature
- Endoscopic retrograde cholangiopancreatography (ERCP) can be used to evaluate very early disease or in patients who cannot tolerate MRI (eg, metal implants, pacemaker)
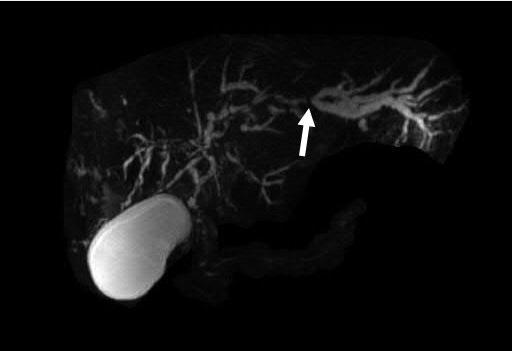
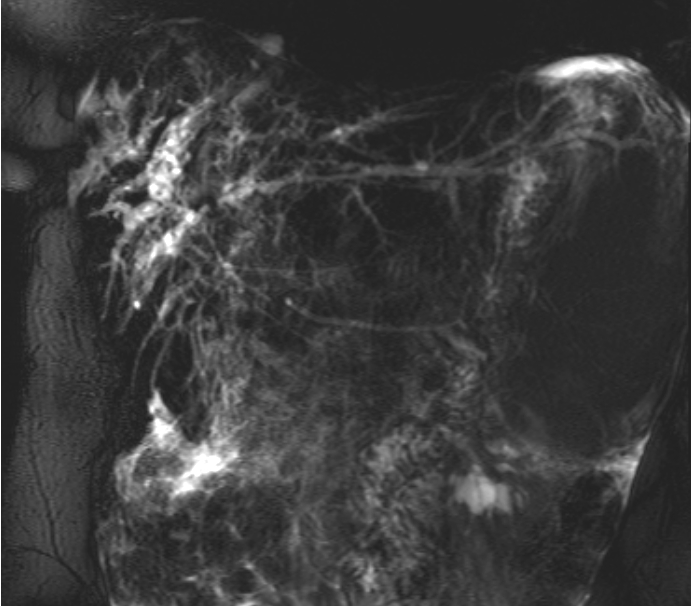 Magnetic resonance cholangiopancreatography showing multifocal intra- and extrahepatic bile-duct stricturing with a dominant left-lobe stricture (arrow) and upstream bile-duct dilation consistent with the diagnosis of primary sclerosing cholangitis.
Magnetic resonance cholangiopancreatography showing multifocal intra- and extrahepatic bile-duct stricturing with a dominant left-lobe stricture (arrow) and upstream bile-duct dilation consistent with the diagnosis of primary sclerosing cholangitis.
In most patients, PSC presents as a stricturing process in the medium to large bile ducts, readily identifiable by MR cholangiopancreatography (alternating strictures and dilations resulting in a “string of beads” pattern). However, a minority of patients may present with involvement of only the small bile ducts, called small-duct PSC. The cholangiogram is normal in these patients; the diagnosis of small-duct PSC can only be made by liver biopsy. Small-duct PSC is associated with a better prognosis than typical PSC, although 10% to 20% of patients with small-duct PSC eventually develop changes in the medium and large ducts.
Liver biopsies are rarely diagnostic; the specific histologic finding of an "onion skin" pattern of fibrous obliteration is seen in a minority of patients. In most cases (>98% in one study), biopsy results do not change management; biopsies are typically reserved for patients with high suspicion for small duct PSC (ie, characteristic histologic findings with normal cholangiographic findings) or an overlap syndrome (Choice D).
PSC often requires liver transplantation and has the highest case-based mortality rate among the autoimmune liver diseases. Median transplant-free survival for patients with PSC is 12 years. There is no current medical therapy for PSC. ERCP to dilate strictures and remove stones is used in symptomatic patients.
Liver transplantation should be considered for patients with decompensated cirrhosis, recurrent bacterial cholangitis, and hilar cholangiocarcinoma. Transplant outcomes for patients with PSC are excellent, with 1-year survival rates of at least 90% and recurrence rates of approximately 20% at 5 years after liver transplantation.
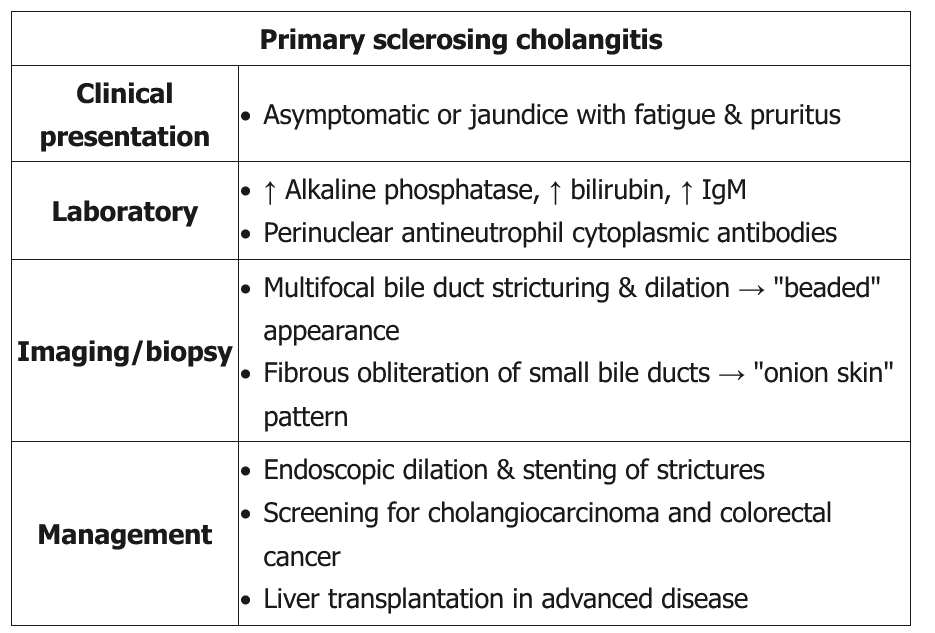
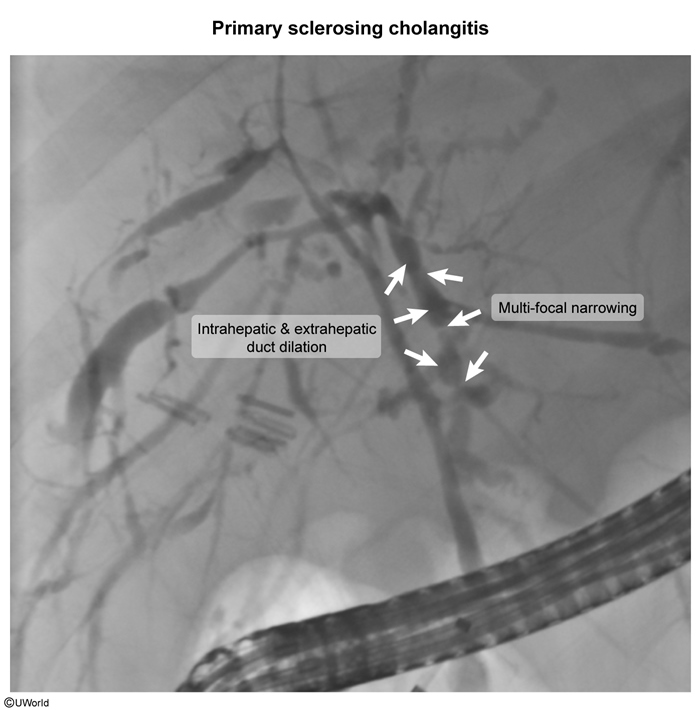
Most patients with PSC are fairly asymptomatic at presentation, and the disease is often detected initially by laboratory abnormalities. If symptoms do occur, fatigue and pruritus are most common. The diagnosis of PSC is usually confirmed with endoscopic cholangiography, which demonstrates multifocal areas of stricture and dilatation of the intra- and extrahepatic bile ducts. MRCP is an alternative study with the advantage of being less invasive.
This patient's presentation is consistent with cholestasis due to primary sclerosing cholangitis (PSC), which is associated with underlying inflammatory bowel disease (IBD) (usually ulcerative colitis) in nearly 90% of patients. PSC is a chronic progressive disorder of unknown etiology with inflammation, fibrosis, and stricturing, most commonly of medium and large biliary ducts.
Patients are usually asymptomatic but can present with fatigue, pruritus, and a cholestatic pattern of elevations in liver function tests. Continued bile duct destruction leads to end-stage liver disease and portal hypertension. Ultrasound is usually nondiagnostic; a cholangiogram (either endoscopic or magnetic resonance) may show multifocal narrowing and dilation of both intrahepatic and extrahepatic bile ducts. Liver biopsy is helpful for disease staging and prognosis, and can reveal intrahepatic ductal obliteration with moderate lymphocytic infiltration and periductal "onion skin" fibrosis.
PSC patients with IBD are at significantly increased risk of colorectal cancer. Current guidelines recommend colonoscopy with full biopsies in newly diagnosed patients with PSC regardless of the presence of other symptoms. Patients found to have IBD require yearly follow-up with colonoscopy; those with PSC but without IBD should have colonoscopy every 5 years. Liver transplantation is the preferred treatment for PSC as medical therapy (eg, cyclosporine) does not appear to slow progression of the disease (Choice B).
Although glucocorticoids are an important treatment for IgG4-related cholangitis, they have not been shown to improve survival in PSC and can worsen bone loss.
Ursodeoxycholic acid is a mainstay of treatment for primary biliary cholangitis (PBC), which can present similarly to PSC. However, PBC usually affects women (90% of cases), and biopsy shows mononuclear cell-mediated destruction and/or periductal granulomatous inflammation of intrahepatic bile ducts. Ursodeoxycholic acid does not have a clear role in management of PSC.